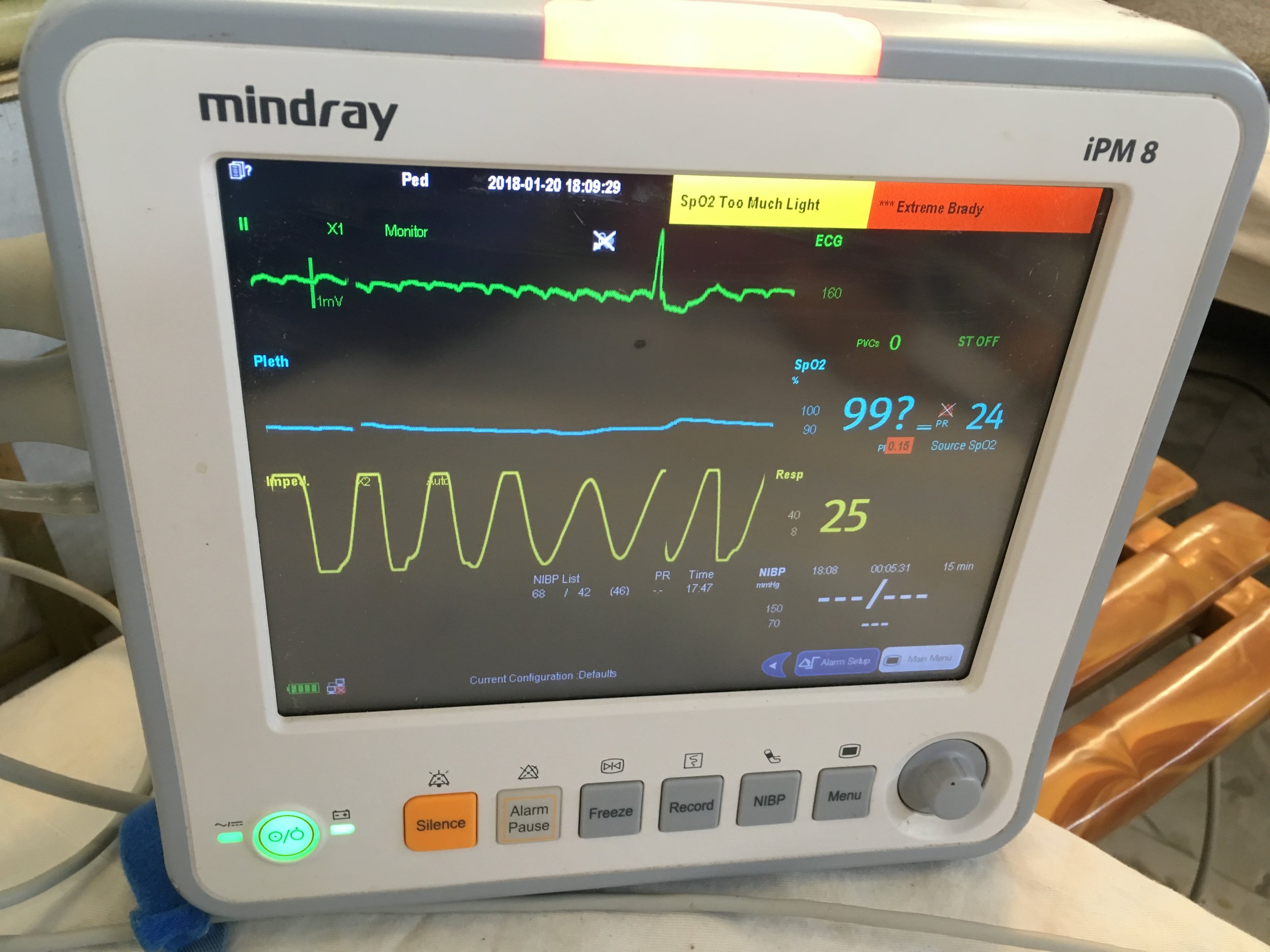
I was woken this morning to the call for prayer as usual at 5.30am, managed another 40 winks then up for breakfast and the usual chaotic drive to the clinic. Today was a fairly quiet day, it’s friday the holy day... around 4pm in comes a wee 4 year old who we had already treated two days ago with the anti toxin for diphtheria... she was floppy, very dry and had sats of 99 but a heart rate of 30. I didn’t quite believe it at first but listening in it sounded about right and on a monitor she had flutter waves with regular escape beats. We gave her a fluid bolus and after a lot of phone calls we transferred her to the MSF centre. Realistically they don’t have a lot more equipment than we do and in hindsight we probably should have just kept her. She had bloods with a creatinine of 700 and never produced any urine despite trying frusemide and I just heard that she died yesterday. Very sad and to think how little we were able to do for her and how much expertise would have been available in the UK. I guess this is what humanitarian work is. At least she was comfortable and with her family at the end.
Today we have had a surge of mumps cases. It seems there’s another outbreak. The WHO have vaccinated for measles and rubella but missed the mumps. The local population aren’t vaccinated for mumps and politically it’s seen as inappropriate to provide better care for the refugees than is provided by the government for the local people. Seems crazy! And I wonder how many host locals will end up with mumps.. we’ll see. Trouble is the ‘bull neck’ of diphtheria can look just like bilateral mumps and even the google images use the same photos for both! With no diagnostic facilities this makes deciding who to treat with the toxic horse serum for diphtheria very tricky. We are seeing the face of a changing outbreak every day and are learning and adapting with it. The team really comes together here. The epidemiologists are working hard to track the outbreak, organising data trying to work out what the treatment effects are and how good our case definition is. Hopefully we get it right most of the time.
I had my first 24 hour shift yesterday.. it definitely makes you feel slightly vulnerable when you are left with your buddy in the middle of a refugee camp. The security guys are always available on the phone and it is reassuring to know that the would come running if we needed them. The background noise is quite something with tannoys blaring, tuc tucs honking, people cramped close together and the regular prayer call.. army ration packs keep us going and the thought of a donut handover as the day team arrive. At least we’ve got a kettle now and can make a decent brew (tetley of course).
A walk on the beach later is a real treat. Time to chill out for an afternoon before starting back tomorrow....
Second day back at AA clinic. We are running 3 treatment centres in total and the docs rotate.. it’s been a fairly busy day with 83 triages and 3 anti toxin treatments.. still two to do. Only one clinic stays open at night so we were about to transfer two patients when we were informed of a demonstration of two groups in the camp- the Rohingya who are demonstrating about plans for repatriation back to Myanmar and the Bangladeshi who want their land back.. you can see the difficulties. The refugees have no where to go and their home is not safe. They would rather stay here where there is food, water and health care. The host nation however understandably are not happy. This is a tourist area and farming land has been used for the camp, never mind the influx of disease and the use of precious resources. Even the elephants are protesting with two reported attacks, this was their land too!!
Either way it was thought not to be safe and we left camp mid afternoon.. no overnight treatment tonight... but at least we are all safe.
I have my 24 hour shift tomorrow... hopefully it will be less eventful..
Rachel x